breast cancer
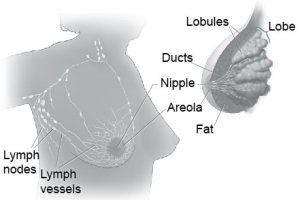
Fig 1. Female breast anatomy.

Fig 2. Ductal carcinoma in situ.

Fig 3. Invasive duct cancer.
Breast cancer is cancer that forms in tissues of the breast,
usually the ducts (tubes that carry milk to
the nipple) and lobules (glands that make milk). It occurs in both men and
women, although male breast cancer is rare.
The breasts also contain lymph vessels. These vessels lead to small, round organs called lymph nodes. Groups of lymph nodes are near the breast in the axilla (underarm), above the collarbone, in the chest behind the breastbone, and in many other parts of the body. The lymph nodes trap bacteria, cancer cells, or other harmful substances.
Research has shown that women with certain risk factors are more likely than others to develop breast cancer. A risk factor is something that may increase the chance of developing a disease.
Studies have found the following risk factors for breast cancer: Age. The chance of getting breast cancer goes up as a woman
gets older. Most cases of breast cancer occur in women over 60. This
disease is not common before menopause.
Personal history of breast cancer. A woman who had breast cancer
in one breast has an increased risk of getting cancer in her other breast.
Family history. A woman's risk of breast cancer is higher if
her mother, sister, or daughter had breast cancer. The risk is higher
if her family member got breast cancer before age 40. Having other relatives
with breast cancer (in either her mother's or father's family) may also
increase a woman's risk.
Certain breast changes. Some women have cells in the breast
that look abnormal under a microscope. Having certain types of abnormal
cells (atypical hyperplasia and lobular carcinoma in situ [LCIS]) increases
the risk of breast cancer.
Gene changes. Changes in certain genes increase the risk of
breast cancer. These genes include BRCA1, BRCA2, and others. Tests can
sometimes show the presence of specific gene changes in families with
many women who have had breast cancer. Health care providers may suggest
ways to try to reduce the risk of breast cancer, or to improve the detection
of this disease in women who have these changes in their genes. NCI
offers publications on gene testing.
Reproductive and menstrual history:
The older a woman is when she has her first child, the greater her chance of breast cancer.
Women who had their first menstrual period before age 12 are at an increased risk of breast cancer.
Women who went through menopause after age 55 are at an increased risk of breast cancer.
Women who never had children are at an increased risk of breast cancer.
Women who take menopausal hormone therapy with estrogen plus progestin after menopause also appear to have an increased risk of breast cancer.
Large, well-designed studies have shown no link between abortion or miscarriage and breast cancer.
Race. Breast cancer is diagnosed more often in white women
than Latina, Asian, or African American women.
Radiation therapy to the chest. Women who had radiation therapy
to the chest (including breasts) before age 30 are at an increased risk
of breast cancer. This includes women treated with radiation for Hodgkin's
lymphoma. Studies show that the younger a woman was when she received
radiation treatment, the higher her risk of breast cancer later in life.
Breast density. Breast tissue may be dense or fatty. Older
women whose mammograms (breast X-rays)
show more dense tissue are at increased risk of breast cancer.
Taking DES (diethylstilbestrol). DES was given to some pregnant
women in the United States between about 1940 and 1971. (It is no longer
given to pregnant women.) Women who took DES during pregnancy may have
a slightly increased risk of breast cancer. The possible effects on
their daughters are under study.
Being overweight or obese after menopause. The chance of getting
breast cancer after menopause is higher in women who are overweight
or obese.
Lack of physical activity. Women who are physically inactive
throughout life may have an increased risk of breast cancer. Being active
may help reduce risk by preventing weight gain and obesity.
Drinking alcohol. Studies suggest that the more alcohol a woman
drinks, the greater her risk of breast cancer.
Many risk factors can be avoided. Others, such as family history, cannot be avoided. Women can help protect themselves by staying away from known risk factors whenever possible.
But it is also important to keep in mind that most women who have known risk factors do not get breast cancer. Also, most women with breast cancer do not have a family history of the disease. In fact, except for growing older, most women with breast cancer have no clear risk factors.
If you think you may be at risk, you should discuss this concern with your doctor. Your doctor may be able to suggest ways to reduce your risk and can plan a schedule for checkups.
Your doctor may suggest the following screening tests for breast cancer:Screening mammogram
Clinical breast exam
Breast self-exam
Women in their 40s and older should have mammograms every 1 to 2 years.
A mammogram is a picture of the breast made with X-rays.
Women who are younger than 40 and have risk factors for breast cancer
should ask their health care provider whether to have mammograms and
how often to have them.
If an abnormal area shows up on your mammogram, you may need to have more x-rays. You also may need a biopsy. A biopsy is the only way to tell for sure if cancer is present. (The "Diagnosis" section has more information on biopsy.)
Mammograms are the best tool doctors have to find breast cancer early. However, mammograms are not perfect:A mammogram may miss some cancers. (The result is called a "false
negative.")
A mammogram may show things that turn out not to be cancer. (The result
is called a "false positive.")
Some fast-growing tumors may grow large or spread to other parts of
the body before a mammogram detects them.
Your health care provider looks for differences in size or shape between your breasts. The skin of your breasts is checked for a rash, dimpling, or other abnormal signs. Your nipples may be squeezed to check for fluid.
Using the pads of the fingers to feel for lumps, your health care provider checks your entire breast, underarm, and collarbone area. A lump is generally the size of a pea before anyone can feel it. The exam is done on one side, then the other. Your health care provider checks the lymph nodes near the breast to see if they are enlarged.
A thorough clinical breast exam may take about 10 minutes.
You should contact your health care provider if you notice any unusual changes in your breasts.
Breast self-exams cannot replace regular screening mammograms and clinical breast exams. Studies have not shown that breast self-exams alone reduce the number of deaths from breast cancer.
You may want to ask the doctor the following questions about screening:Which tests do you recommend for me? Why?
Do the tests hurt? Are there any risks?
How much do mammograms cost? Will my health insurance pay for them?
How soon after the mammogram will I learn the results?
A change in how the breast or nipple feels
A lump or thickening in or near the breast or in the underarm area
Nipple tenderness
A change in how the breast or nipple looks
A change in the size or shape of the breast
A nipple turned inward into the breast
The skin of the breast, areola, or nipple may be scaly, red, or swollen.
It may have ridges or pitting so that it looks like the skin of an orange.
Nipple discharge (fluid)
Some suspicious areas can be seen on a mammogram but cannot be felt during a clinical breast exam. Doctors can use imaging procedures to help see the area and remove tissue. Such procedures include ultrasound-guided, needle-localized, or stereotactic biopsy.
Doctors can remove tissue from the breast in different ways:Fine-needle aspiration. Your doctor uses a thin needle to remove
fluid from a breast lump. If the fluid appears to contain cells, a pathologist
at a lab checks them for cancer with a microscope. If the fluid is clear,
it may not need to be checked by a lab.
Core biopsy. Your doctor uses a thick needle to remove breast
tissue. A pathologist checks for cancer cells. This procedure is also
called a needle biopsy.
Surgical biopsy. Your surgeon removes a sample of tissue. A
pathologist checks the tissue for cancer cells.
An incisional biopsy takes a sample of a lump or abnormal area.
An excisional biopsy takes the entire lump or area.
You may want to ask your doctor the following questions before having a biopsy: What kind of biopsy will I have? Why?
How long will it take? Will I be awake? Will it hurt? Will I have anesthesia? What kind?
Are there any risks? What are the chances of infection or bleeding
after the biopsy?
How soon will I know the results?
If I do have cancer, who will talk with me about the next steps? When?
Hormone receptor test. This test shows whether the tissue has
certain hormone receptors. Tissue with these receptors needs hormones
(estrogen or progesterone) to grow.
HER2 test. This test shows whether the tissue has a protein
called human epidermal growth factor receptor-2 (HER2) or the HER2/neu
gene. Having too much protein or too many copies of the gene in the
tissue may increase the chance that the breast cancer will come back
after treatment.
These are the stages of breast cancer: Stage 0 is carcinoma in situ. The cancer cells are
found only on the surface of the inner lining of the bladder. The doctor
may call this superficial cancer or carcinoma in situ.
Lobular carcinoma in situ (LCIS). Abnormal cells are in the lining of a lobule. LCIS seldom becomes invasive cancer. However, having LCIS in one breast increases the risk of cancer for both breasts.
Ductal carcinoma in situ (DCIS). Abnormal cells are in the lining of a duct. DCIS is also called intraductal carcinoma (Figure 2). The abnormal cells have not spread outside the duct. They have not invaded the nearby breast tissue. DCIS sometimes becomes invasive cancer if not treated.
Stage I is an early stage of invasive breast cance (Figure 3)r.
The tumor is no more than 2 centimeters (three-quarters of an inch)
across. Cancer cells have not spread beyond the breast.
Stage II is one of the following:
The tumor is between 2 and 5 centimeters (three-quarters of an inch to 2 inches). The cancer may have spread to the lymph nodes under the arm.
The tumor is larger than 5 centimeters (2 inches). The cancer has not spread to the lymph nodes under the arm.
Stage III may be a large tumor, but the cancer has
not spread beyond the breast and nearby lymph nodes. It is locally advanced
cancer.
Stage IIIA is one of the following:
The tumor is more than 5 centimeters across. The cancer has spread to the underarm lymph nodes.
Stage IIIB is one of the following:
The tumor has grown into the chest wall or the skin of the breast.
The cancer has spread to lymph nodes behind the breastbone.
Inflammatory breast cancer is a rare type of Stage IIIB breast cancer. The breast looks red and swollen because cancer cells block the lymph vessels in the skin of the breast.
Stage IIIC is a tumor of any size. It has spread
in one of the following ways:
The cancer has spread to the lymph nodes under or above the collarbone.
Stage IV is distant metastatic cancer. The cancer
has spread to other parts of the body.
The breast
The breasts sit on the chest muscles that cover the ribs. Each breast is made of 15 to 20 lobes. Lobes contain many smaller lobules. Lobules contain groups of tiny glands, called mammary glands, that can produce milk. Milk flows from the lobules through thin tubes called ducts to the nipple. The nipple is in the center of a dark area of skin called the areola. Fat fills the spaces between the lobules and ducts.The breasts also contain lymph vessels. These vessels lead to small, round organs called lymph nodes. Groups of lymph nodes are near the breast in the axilla (underarm), above the collarbone, in the chest behind the breastbone, and in many other parts of the body. The lymph nodes trap bacteria, cancer cells, or other harmful substances.
Risk factors
No one knows the exact causes of breast cancer. Doctors often cannot explain why one woman develops breast cancer and another does not. They do know that bumping, bruising, or touching the breast does not cause cancer. And breast cancer is not contagious. You cannot "catch" it from another person.Research has shown that women with certain risk factors are more likely than others to develop breast cancer. A risk factor is something that may increase the chance of developing a disease.
Studies have found the following risk factors for breast cancer:
The older a woman is when she has her first child, the greater her chance of breast cancer.
Women who had their first menstrual period before age 12 are at an increased risk of breast cancer.
Women who went through menopause after age 55 are at an increased risk of breast cancer.
Women who never had children are at an increased risk of breast cancer.
Women who take menopausal hormone therapy with estrogen plus progestin after menopause also appear to have an increased risk of breast cancer.
Large, well-designed studies have shown no link between abortion or miscarriage and breast cancer.
Other possible risk factors are under study. Researchers are studying the effect of diet, physical activity, and genetics on breast cancer risk. They are also studying whether certain substances in the environment can increase the risk of breast cancer.
Many risk factors can be avoided. Others, such as family history, cannot be avoided. Women can help protect themselves by staying away from known risk factors whenever possible.
But it is also important to keep in mind that most women who have known risk factors do not get breast cancer. Also, most women with breast cancer do not have a family history of the disease. In fact, except for growing older, most women with breast cancer have no clear risk factors.
If you think you may be at risk, you should discuss this concern with your doctor. Your doctor may be able to suggest ways to reduce your risk and can plan a schedule for checkups.
Screening
Screening for breast cancer before there are symptoms can be important. Screening can help doctors find and treat cancer early. Treatment is more likely to work well when cancer is found early.Your doctor may suggest the following screening tests for breast cancer:
You should ask your doctor about when to start and how often to check for breast cancer.
Screening mammogram
To find breast cancer early, NCI recommends that:
Mammograms can often show a breast lump before it can be felt. They also can show a cluster of tiny specks of calcium. These specks are called microcalcifications. Lumps or specks can be from cancer, precancerous cells, or other conditions. Further tests are needed to find out if abnormal cells are present.
If an abnormal area shows up on your mammogram, you may need to have more x-rays. You also may need a biopsy. A biopsy is the only way to tell for sure if cancer is present. (The "Diagnosis" section has more information on biopsy.)
Mammograms are the best tool doctors have to find breast cancer early. However, mammograms are not perfect:
Mammograms (as well as dental X-rays, and other routine X-rays) use very small doses of radiation. The risk of any harm is very slight, but repeated X-rays could cause problems. The benefits nearly always outweigh the risk. You should talk with your health care provider about the need for each X-ray. You should also ask for shields to protect parts of your body that are not in the picture.
Clinical breast exam
During a clinical breast exam, your health care provider checks your breasts. You may be asked to raise your arms over your head, let them hang by your sides, or press your hands against your hips.Your health care provider looks for differences in size or shape between your breasts. The skin of your breasts is checked for a rash, dimpling, or other abnormal signs. Your nipples may be squeezed to check for fluid.
Using the pads of the fingers to feel for lumps, your health care provider checks your entire breast, underarm, and collarbone area. A lump is generally the size of a pea before anyone can feel it. The exam is done on one side, then the other. Your health care provider checks the lymph nodes near the breast to see if they are enlarged.
A thorough clinical breast exam may take about 10 minutes.
Breast self-exam
You may perform monthly breast self-exams to check for any changes in your breasts. It is important to remember that changes can occur because of aging, your menstrual cycle, pregnancy, menopause, or taking birth control pills or other hormones. It is normal for breasts to feel a little lumpy and uneven. Also, it is common for your breasts to be swollen and tender right before or during your menstrual period.You should contact your health care provider if you notice any unusual changes in your breasts.
Breast self-exams cannot replace regular screening mammograms and clinical breast exams. Studies have not shown that breast self-exams alone reduce the number of deaths from breast cancer.
You may want to ask the doctor the following questions about screening:
If the results show a problem, how will you learn if I have cancer?
Symptoms of breast cancer
Common symptoms of breast cancer include:
Early breast cancer usually does not cause pain. Still, a woman should see her health care provider about breast pain or any other symptom that does not go away. Most often, these symptoms are not due to cancer. Other health problems may also cause them. Any woman with these symptoms should tell her doctor so that problems can be diagnosed and treated as early as possible.
Diagnosis
If you have a symptom or screening test result that suggests cancer, your doctor must find out whether it is due to cancer or to some other cause. Your doctor may ask about your personal and family medical history. You may have a physical exam. Your doctor also may order a mammogram or other imaging procedure. These tests make pictures of tissues inside the breast. After the tests, your doctor may decide no other exams are needed. Your doctor may suggest that you have a follow-up exam later on. Or you may need to have a biopsy to look for cancer cells.Clinical breast exam
Your health care provider feels each breast for lumps and looks for other problems. If you have a lump, your doctor will feel its size, shape, and texture. Your doctor will also check to see if it moves easily. Benign lumps often feel different from cancerous ones. Lumps that are soft, smooth, round, and movable are likely to be benign. A hard, oddly shaped lump that feels firmly attached within the breast is more likely to be cancer.Diagnostic mammogram
Diagnostic mammograms are x-ray pictures of the breast. They take clearer, more detailed images of areas that look abnormal on a screening mammogram. Doctors use them to learn more about unusual breast changes, such as a lump, pain, thickening, nipple discharge, or change in breast size or shape. Diagnostic mammograms may focus on a specific area of the breast. They may involve special techniques and more views than screening mammograms.Ultrasound
An ultrasound device sends out sound waves that people cannot hear. The waves bounce off tissues. A computer uses the echoes to create a picture. Your doctor can view these pictures on a monitor. The pictures may show whether a lump is solid or filled with fluid. A cyst is a fluid-filled sac. Cysts are not cancer. But a solid mass may be cancer. After the test, your doctor can store the pictures on video or print them out. This exam may be used along with a mammogram.Magnetic resonance imaging
Magnetic resonance imaging (MRI) uses a powerful magnet linked to a computer. MRI makes detailed pictures of breast tissue. Your doctor can view these pictures on a monitor or print them on film. MRI may be used along with a mammogram.Biopsy
Your doctor may refer you to a surgeon or breast disease specialist for a biopsy. Fluid or tissue is removed from your breast to help find out if there is cancer.Some suspicious areas can be seen on a mammogram but cannot be felt during a clinical breast exam. Doctors can use imaging procedures to help see the area and remove tissue. Such procedures include ultrasound-guided, needle-localized, or stereotactic biopsy.
Doctors can remove tissue from the breast in different ways:
An excisional biopsy takes the entire lump or area.
If cancer cells are found, the pathologist can tell what kind of cancer it is. The most common type of breast cancer is ductal carcinoma. Abnormal cells are found in the lining of the ducts. Lobular carcinoma is another type. Abnormal cells are found in the lobules.
You may want to ask your doctor the following questions before having a biopsy:
Additional tests
If you are diagnosed with cancer, your doctor may order special lab tests on the breast tissue that was removed. These tests help your doctor learn more about the cancer and plan treatment:
Staging the disease
To plan your treatment, your doctor needs to know the extent (stage) of the disease. The stage is based on the size of the tumor and whether the cancer has spread. Staging may involve x-rays and lab tests. These tests can show whether the cancer has spread and, if so, to what parts of your body. When breast cancer spreads, cancer cells are often found in lymph nodes under the arm (axillary lymph nodes). The stage often is not known until after surgery to remove the tumor in your breast and the lymph nodes under your arm.These are the stages of breast cancer:
Lobular carcinoma in situ (LCIS). Abnormal cells are in the lining of a lobule. LCIS seldom becomes invasive cancer. However, having LCIS in one breast increases the risk of cancer for both breasts.
Ductal carcinoma in situ (DCIS). Abnormal cells are in the lining of a duct. DCIS is also called intraductal carcinoma (Figure 2). The abnormal cells have not spread outside the duct. They have not invaded the nearby breast tissue. DCIS sometimes becomes invasive cancer if not treated.
The tumor in the breast is no more than 2 centimeters (three-quarters of an inch) across. The cancer has spread to the lymph nodes under the arm.
The tumor is between 2 and 5 centimeters (three-quarters of an inch to 2 inches). The cancer may have spread to the lymph nodes under the arm.
The tumor is larger than 5 centimeters (2 inches). The cancer has not spread to the lymph nodes under the arm.
The tumor in the breast is smaller than 5 centimeters (2 inches). The cancer has spread to underarm lymph nodes that are attached to each other or to other structures.
The tumor is more than 5 centimeters across. The cancer has spread to the underarm lymph nodes.
The tumor has grown into the chest wall or the skin of the breast.
The cancer has spread to lymph nodes behind the breastbone.
Inflammatory breast cancer is a rare type of Stage IIIB breast cancer. The breast looks red and swollen because cancer cells block the lymph vessels in the skin of the breast.
The cancer has spread to the lymph nodes behind the breastbone and under the arm.
The cancer has spread to the lymph nodes under or above the collarbone.
Recurrent cancer is cancer that has come back (recurred) after a period of time when it could not be detected. It may recur locally in the breast or chest wall. Or it may recur in any other part of the body, such as the bone, liver, or lungs.


