vitamin A
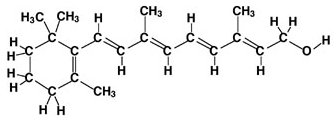
Retinol (vitamin A).
Vitamin A is a group of compounds that play an important role in the healthy functioning of the eye, bone growth, reproduction, cell division, and cell differentiation (in which a cell becomes part of the brain, muscle, lungs, blood, or other specialized tissue.) Vitamin A helps regulate the immune system, which helps prevent or fight off infections by making white blood cells that destroy harmful bacteria and viruses. It also may help lymphocytes (a type of white blood cell) fight infections more effectively.
Vitamin A promotes healthy surface linings of the eyes and the respiratory, urinary, and intestinal tracts. When those linings break down, it becomes easier for bacteria to enter the body and cause infection. Vitamin A also helps the skin and mucous membranes function as a barrier to bacteria and viruses.
In general, there are two categories of vitamin A, depending on whether the food source is an animal or a plant.
Vitamin A found in foods that come from animals is called preformed vitamin A. It is absorbed in the form of retinol, one of the most usable (active) forms of vitamin A. Sources include liver, whole milk, and some fortified food products. Retinol can be made into retinal and retinoic acid (other active forms of vitamin A) in the body.
Vitamin A that is found in colorful fruits and vegetables is called provitamin
A carotenoid. They can be made into retinol
in the body. In the United States, approximately 26% of vitamin A consumed
by men and 34% of vitamin A consumed by women is in the form of provitamin
A carotenoids. Common provitamin A carotenoids found in foods that come
from plants are beta-carotene, alpha-carotene, and beta-cryptoxanthin. Among
these, beta-carotene is most efficiently made into retinol. Alpha-carotene
and beta-cryptoxanthin are also converted to vitamin A, but only half as
efficiently as beta-carotene.
Of the 563 identified carotenoids, fewer than 10% can be made into vitamin A in the body. Lycopene, lutein, and zeaxanthin are carotenoids that do not have vitamin A activity but have other health promoting properties.
Some provitamin A carotenoids have been shown to function as antioxidants in laboratory studies; however, this role has not been consistently demonstrated in humans. Antioxidants protect cells from free radicals, which are potentially damaging by-products of oxygen metabolism that may contribute to the development of some chronic diseases.
Dietary sources of vitamin A
Retinol is found in foods that come from animals such as whole eggs, milk, and liver. Most fat-free milk and dried nonfat milk solids sold in the United States are fortified with vitamin A to replace the amount lost when the fat is removed. Fortified foods such as fortified breakfast cereals also provide vitamin A. Provitamin A carotenoids are abundant in darkly colored fruits and vegetables. The 2000 National Health and Nutrition Examination Survey indicated that major dietary contributors of retinol are milk, margarine, eggs, beef liver and fortified breakfast cereals, whereas major contributors of provitamin A carotenoids are carrots, cantaloupes, sweet potatoes, and spinach.
Vitamin A in foods that come from animals is well absorbed and used efficiently by the body. Vitamin A in foods that come from plants is not as well absorbed as animal sources of vitamin A.
Vitamin A deficiency
Vitamin A deficiency is common in developing countries but rarely seen in the United States. Approximately 250,000 to 500,000 malnourished children in the developing world become blind each year from a deficiency of vitamin A. In the United States, vitamin A deficiency is most often associated with strict dietary restrictions and excess alcohol intake. Severe zinc deficiency, which is also associated with strict dietary limitations, often accompanies vitamin A deficiency. Zinc is required to make retinol binding protein (RBP) which transports vitamin A. Therefore, a deficiency in zinc limits the body's ability to move vitamin A stores from the liver to body tissues.
Night blindness is one of the first signs of vitamin A deficiency. In ancient Egypt, it was known that night blindness could be cured by eating liver, which was later found to be a rich source of the vitamin. Vitamin A deficiency contributes to blindness by making the cornea very dry and damaging the retina and cornea.
Vitamin A deficiency diminishes the ability to fight infections. In countries where such deficiency is common and immunization programs are limited, millions of children die each year from complications of infectious diseases such as measles. In vitamin A-deficient individuals, cells lining the lungs lose their ability to remove disease-causing microorganisms. This may contribute to the pneumonia associated with vitamin A deficiency.
There is increased interest in early forms of vitamin A deficiency, described as low storage levels of vitamin A that do not cause obvious deficiency symptoms. This mild degree of vitamin A deficiency may increase children's risk of developing respiratory and diarrheal infections, decrease growth rate, slow bone development, and decrease likelihood of survival from serious illness. Children in the United States who are considered to be at increased risk for subclinical vitamin A deficiency include:
A deficiency can occur when vitamin A is lost through chronic diarrhea and through an overall inadequate intake, as is often seen with protein-energy malnutrition. Low blood retinol concentrations indicate depleted levels of vitamin A. This occurs with vitamin A deficiency but also can result from an inadequate intake of protein, calories, and zinc, since these nutrients are needed to make RBP. Iron deficiency can also affect vitamin A metabolism, and iron supplements provided to iron-deficient individuals may improve body stores of vitamin A and iron.
Excess alcohol intake depletes vitamin A stores. Also, diets high in alcohol often do not provide recommended amounts of vitamin A. It is very important for people who consume excessive amounts of alcohol to include good sources of vitamin A in their diets. Vitamin A supplements may not be recommended for individuals who abuse alcohol, however, because their livers may be more susceptible to potential toxicity from high doses of vitamin A. A medical doctor will need to evaluate this situation and determine the need for vitamin A supplements.
Who may need extra vitamin A to prevent deficiency?
The World Health Organization (WHO) and the United Nations Children's Fund (UNICEF) recommend vitamin A administration for all children diagnosed with measles in communities where vitamin A deficiency is a serious problem and where death from measles is greater than 1%. In 1994, the American Academy of Pediatrics recommended vitamin A supplements for two subgroups of children likely to be at high risk for subclinical vitamin A deficiency: children aged 6 months to 24 months who are hospitalized with measles, and hospitalized children older than 6 months.
Fat malabsorption can result in diarrhea and prevent normal absorption of vitamin A. Over time this may result in vitamin A deficiency. Those conditions include:
Healthy adults usually have a reserve of vitamin A stored in their livers and should not be at risk of deficiency during periods of temporary or short-term fat malabsorption. Long-term problems absorbing fat, however, may result in deficiency. In these instances physicians may recommend additional vitamin A.
Vegetarians who do not consume eggs and dairy foods need provitamin A carotenoids to meet their need for vitamin A. They should include a minimum of five servings of fruits and vegetables in their daily diet and regularly choose dark green leafy vegetables and orange and yellow fruits to consume recommended amounts of vitamin A.
Current issues and controversies
Vitamin A, beta carotene, and cancer
Dietary intake studies suggest an association between diets rich in beta-carotene and vitamin A and a lower risk of many types of cancer. A higher intake of green and yellow vegetables or other food sources of beta carotene and/or vitamin A may decrease the risk of lung cancer. However, a number of studies that tested the role of beta-carotene supplements in cancer prevention did not find them to protect against the disease. In the Alpha-Tocopherol Beta-Carotene (ATBC) Cancer Prevention Study, more than 29,000 men who regularly smoked cigarettes were randomized to receive 20 mg beta-carotene alone, 50 mg alpha-tocopherol alone, supplements of both, or a placebo for 5 to 8 years. Incidence of lung cancer was 18% higher among men who took the beta-carotene supplement. Eight percent more men in this group died, as compared to those receiving other treatments or placebo. Similar results were seen in the Carotene and Retinol Efficacy Trial (CARET), a lung cancer chemoprevention study that provided subjects with supplements of 30 mg beta-carotene and 25,000 IU retinyl palmitate (a form of vitamin A) or a placebo. This study was stopped after researchers discovered that subjects receiving beta-carotene had a 46% higher risk of dying from lung cancer.
The IOM states that "beta-carotene supplements are not advisable for the general population," although they also state that this advice "does not pertain to the possible use of supplemental beta-carotene as a provitamin A source for the prevention of vitamin A deficiency in populations with inadequate vitamin A".
Vitamin A and osteoporosis
Osteoporosis, a disorder characterized by porous and weak bones, is a serious health problem for more than 10 million Americans, 80% of whom are women. Another 18 million Americans have decreased bone density which precedes the development of osteoporosis. Many factors increase the risk for developing osteoporosis, including being female, thin, inactive, at advanced age, and having a family history of osteoporosis. An inadequate dietary intake of calcium, cigarette smoking, and excessive intake of alcohol also increase the risk.
Researchers are now examining a potential new risk factor for osteoporosis: an excess intake of vitamin A. Animal, human, and laboratory research suggests an association between greater vitamin A intake and weaker bones. Worldwide, the highest incidence of osteoporosis occurs in northern Europe, a population with a high intake of vitamin A. However, decreased biosynthesis of vitamin D associated with lower levels of sun exposure in this population may also contribute to this finding.
One small study of nine healthy individuals in Sweden found that the amount of vitamin A in one serving of liver may impair the ability of vitamin D to promote calcium absorption. To further test the association between excess dietary intakes of vitamin A and increased risk for hip fractures, researchers in Sweden compared bone mineral density and retinol intake in approximately 250 women with a first hip fracture to 875 age-matched controls. They found that a dietary retinol intake greater than 1,500 mcg/day (more than twice the recommended intake for women) was associated with reduced bone mineral density and increased risk of hip fracture as compared to women who consumed less than 500 mcg/day.
This issue was also examined by researchers with the Nurses Health Study, who looked at the association between vitamin A intake and hip fractures in over 72,000 postmenopausal women. Women who consumed the most vitamin A in foods and supplements (3,000 mcg or more per day as retinol equivalents, which is over three times the recommended intake) had a significantly increased risk of experiencing a hip fracture as compared to those consuming the least amount (less than 1,250 mcg/day). The effect was lessened by use of estrogens. These observations raise questions about the effect of retinol because retinol intakes greater than 2,000 mcg/day were associated with an increased risk of hip fracture as compared to intakes less than 500 mcg.
A longitudinal study in more than 2,000 Swedish men compared blood levels of retinol to the incidence of fractures in men. The investigators found that the risk of fractures was greatest in men with the highest blood levels of retinol (more than 75 mcg per deciliter [dL]). Men with blood retinol levels in the 99th percentile (greater than 103 mcg per dL) had an overall risk of fracture that exceeded the risk among men with lower levels of retinol by a factor of seven. High vitamin A intake, however, does not necessarily equate to high blood levels of retinol. Age, gender, hormones, and genetics also influence these levels. Researchers did not find any association between blood levels of beta-carotene and risk of hip fracture. Researchers' findings, which are consistent with the results of animal, in vitro (laboratory), and epidemiologic studies, suggest that intakes above the UL, or approximately two times that of the RDA for vitamin A, may pose subtle risks to bone health that require further study.
The Centers for Disease Control and Prevention (CDC) reviewed data from NHANES III (1988-94) to determine whether there was any association between bone mineral density and blood levels of retinyl esters, a form of vitamin A. No significant associations between blood levels of retinyl esters and bone mineral density in 5,800 subjects were found.
There is no evidence of an association between beta-carotene intake, especially from fruits and vegetables, and increased risk of osteoporosis. Current evidence points to a possible association with vitamin A as retinol only. If you have specific questions regarding your intake of vitamin A and risk of osteoporosis, discuss this information with your physician or other qualified healthcare provider to determine what's best for your personal health.
Health risks of too much vitamin A
Hypervitaminosis A refers to high storage levels of vitamin A in the body that can lead to toxic symptoms. There are four major adverse effects of hypervitaminosis A: birth defects, liver abnormalities, reduced bone mineral density that may result in osteoporosis (see the previous section), and central nervous system disorders.
Toxic symptoms can also arise after consuming very large amounts of preformed vitamin A over a short period of time. Signs of acute toxicity include nausea and vomiting, headache, dizziness, blurred vision, and muscular uncoordination. Although hypervitaminosis A can occur when large amounts of liver are regularly consumed, most cases result from taking excess amounts of the nutrient in supplements.
The IOM has established Tolerable Upper Intake Levels (ULs) for vitamin A that apply to healthy populations. The UL was established to help prevent the risk of vitamin A toxicity. The risk of adverse health effects increases at intakes greater than the UL. The UL does not apply to malnourished individuals receiving vitamin A either periodically or through fortification programs as a means of preventing vitamin A deficiency. It also does not apply to individuals being treated with vitamin A by medical doctors for diseases such as retinitis pigmentosa.
Retinoids are compounds that are chemically similar to vitamin A. Over the past 15 years, synthetic retinoids have been prescribed for acne, psoriasis, and other skin disorders. Isotretinoin (Roaccutane® or Accutane®) is considered an effective anti-acne therapy. At very high doses, however, it can be toxic, which is why this medication is usually saved for the most severe forms of acne. The most serious consequence of this medication is birth defects. It is extremely important for sexually active females who may become pregnant and who take these medications to use an effective method of birth control. Women of childbearing age who take these medications are advised to undergo monthly pregnancy tests to make sure they are not pregnant.
Health risks of too many carotenoids
Provitamin A carotenoids such as beta-carotene are generally considered safe because they are not associated with specific adverse health effects. Their conversion to vitamin A decreases when body stores are full. A high intake of provitamin A carotenoids can turn the skin yellow, but this is not considered dangerous to health.
Clinical trials that associated beta-carotene supplements with a greater incidence of lung cancer and death in current smokers raise concerns about the effects of beta-carotene supplements on long-term health; however, conflicting studies make it difficult to interpret the health risk. For example, the Physicians Health Study compared the effects of taking 50 mg beta-carotene every other day to a placebo in over 22,000 male physicians and found no adverse health effects. Also, a trial that tested the ability of four different nutrient combinations to help prevent the development of esophageal and gastric cancers in 30,000 men and women in China suggested that after five years those participants who took a combination of beta-carotene, selenium, and vitamin E had a 13% reduction in cancer deaths. In one lung cancer trial, men who consumed more than 11 grams/day of alcohol (approximately one drink per day) were more likely to show an adverse response to beta-carotene supplements, which may suggest a potential relationship between alcohol and beta-carotene.
The IOM did not set ULs for carotene or other carotenoids. Instead, it concluded that beta-carotene supplements are not advisable for the general population. As stated earlier, however, they may be appropriate as a provitamin A source for the prevention of vitamin A deficiency in specific populations.
Vitamin A intakes and healthful diets
According to the 2005 Dietary Guidelines for Americans, "Nutrient needs should be met primarily through consuming foods. Foods provide an array of nutrients and other compounds that may have beneficial effects on health. In certain cases, fortified foods and dietary supplements may be useful sources of one or more nutrients that otherwise might be consumed in less than recommended amounts. However, dietary supplements, while recommended in some cases, cannot replace a healthful diet.


